A dead tooth is serious, and it’s something anyone with untreated caries can experience if they allow the decay to progress untreated. Statistically, 29.3% of people between the age of 20 and 34 have permanent teeth with caries that are not treated.
If you seek treatment for these caries, you can avoid the risk of root canals or tooth extraction.
However, if you have a tooth that is severely decayed, it may already be dead. We always recommend scheduling an appointment with a dentist to have a dental exam performed immediately.
You can also look for common signs that a tooth is dead, but be warned - even an alive tooth can cause some of the symptoms we’ll mention below.
What Causes a Tooth to Die?

Your teeth are alive. Inside of your tooth, there are nerves, blood vessels and blood. Blood flow to the tooth is responsible for ensuring that the tooth has the minerals it needs to remain healthy. Disruption of this blood flow is one of the key reasons for tooth death. You can disrupt blood flow by:
- Impact injuries
- Falls on the mouth
- Etc.
Many sports players, especially in hockey and football, suffer impact injuries that cause tooth death. Aside from impact-related injuries, your tooth may die from:
- Untreated tooth decay
- Poor dental hygiene
Your permanent teeth do not grow back. If you allow the tooth to rot to a severe extent, there’s a risk that the tooth will die.
Below are some of the symptoms of tooth death that you’ll have an easy time identifying.
Self-Identification of a Dead Tooth
If you experience any of the following, it’s a reason to call our office and schedule an appointment. Your teeth will not heal on their own if the tooth is dead or on the brink of death. The following are signs that the tooth may be dead or dying:
Discoloration
Tooth discoloration means something is wrong with the tooth. You may notice teeth yellowing, which happens to a lot of people, but yellowing is often a sign of poor oral hygiene or smoking. Instead, you’ll want to be on the lookout for teeth that are:
- Gray: A graying tooth is likely lacking proper blood flow and is on the brink of death if it’s not already dead.
- Black: In some patients, their teeth turn black, and this discoloration is a clear indication that the tooth is dead.
- Brown: A brown tooth is similar to the black tooth above and a sign that the tooth needs treatment.
Some patients even have severe yellowing of the tooth that goes beyond just a few shades that we notice with poor oral hygiene.
Your teeth will not turn gray, brown or black unless there is severe tooth decay that goes unchecked for an extended period of time.
Odors
A foul odor from your tooth means that the tooth is either in a severe state of decay or death. Patients that have a dead tooth often report that they experience:
- Bad breath
- Foul tastes in their mouth
Since it’s difficult to pinpoint the cause of the foul odor or taste without an exam, it’s important to have a full examination performed. You may have something else going on that is causing your bad breath, such as halitosis.
Pain or Sensitivity
Tooth pain or sensitivity can happen when your tooth has a cavity or even when the tooth is in a generally healthy state. However, there’s also a chance that the pain is caused by a dying tooth. When tooth death is ongoing, it can cause:
- Sensitivity to hot and cold
- Worsening pain
Pain around the tooth in question or when chewing on the tooth may be a sign of a dead tooth. Unfortunately, even minor forms of decay can cause tooth pain, so there’s no easy way to identify if the pain is from decay or death without an examination.
If you do notice that the tooth is in a severe state of decay and you’re experiencing the symptoms above, it may be tooth death.
Abscess, Swelling and/or Pus
Dying teeth are in severe decay and will often become infected. You may notice that the gums around the teeth are swollen or that an abscess has formed on the gum. An abscess fills with pus and is one of the easiest ways to identify a tooth infection.
You never want to ignore an abscess or swollen gums because you’ll need professional treatment and medication to stop the infection from spreading.
If you’ve ever had root canals performed or had a tooth pulled, you know that the symptoms above can be a result of a non-dead tooth. It’s not uncommon for a patient to come into our office with swollen gums or an abscess and still have their tooth alive.
Anyone noticing the symptoms above should come into our office for a full exam so that we can address the issue.
How Our Team Identifies a Dead Tooth
If you come into our office and we suspect that your tooth is dead, we’ll start with a visual examination of the tooth. We’ll look for many of the signs that we covered in the last section before performing:
- Pulp testing: We can conduct what is known as electric pulp testing to determine if the tooth is or is not valid. The test involves sending an electric pulse into the tooth's root and waiting for a response. If the response is faint or you do not feel anything, there’s a good chance the tooth is dead.
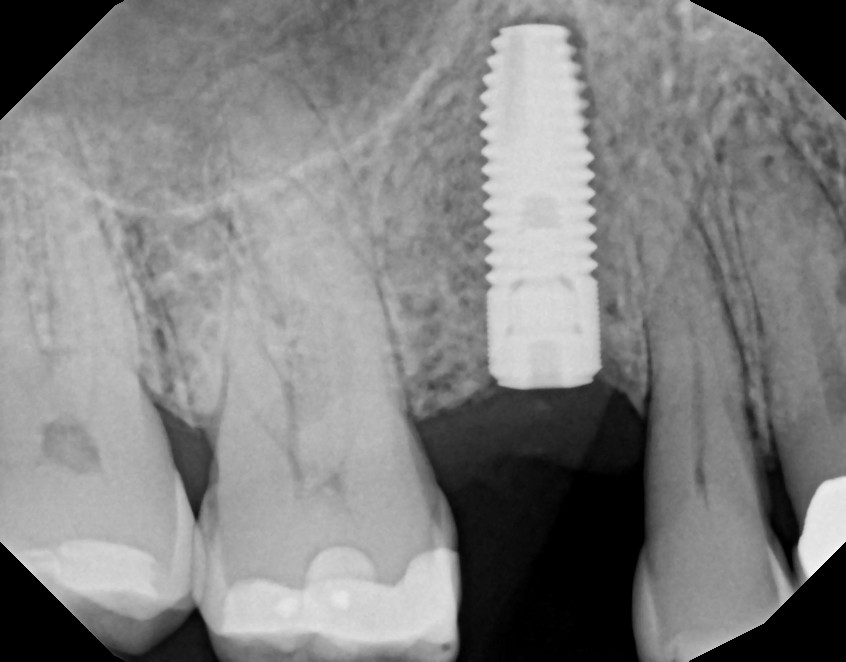
- X-rays: An X-ray may be taken to look for darker colors on the images. When a tooth is dead, the images are often darker and show the extent of tooth decay.

Multiple other tests may be performed in conjunction with one another to determine if your tooth is dead or not. X-rays still remain one of our best methods of judging the level of tooth decay and if the tooth is dead.
Once the dentist understands the underlying issue, we can then work to treat the dead tooth.
Treating a Dead Tooth
Your tooth is dead: now what? We have a few options to treat your tooth that we’ll discuss with you when you’re in our office. The main treatment options that we have include:
Root Canals
Root canals require us to:
- Remove all of the infected tissue from your tooth’s pulp
- Clear out the infection to the best of our ability
- Drill out any of the infected tooth chambers
- Fill in the chambers in the tooth and fill in the hole left behind
- Create a crown of the tooth that matches your bite
- Place the crown
Simple root canals last as few as 30 minutes, but in more severe cases, it can take up to 90 minutes or more to complete root canals.
We always recommend root canals before a tooth extraction because they’re a way to save your existing tooth. You always want to save any tooth that you can because it will have less of an impact on your dental health in the long term.
In severe cases, we may recommend a tooth extraction because there is not enough of the existing tooth left for us to place a crown. The crown that we place will protect the remaining tooth from further decay, but we do need a decent amount of the original tooth to cement the crown in place. We can, in some cases, build the tooth up to allow for a solid foundation to attach the crown.
Tooth Extraction
If the tooth is decayed beyond the point of saving or is fully dead and has been for some time, we’ll have no other option but to extract the tooth. This is a straightforward procedure that requires us to numb the area surrounding the tooth before removing it. If the tooth’s root is below the gum line, we may have to make an incision in the gum to remove the tooth. Incisions will then be stitched up to ensure that your gums heal properly.
Once the tooth is removed, you’ll need to wait up to two weeks for the site of the extraction to heal. Most of our patients can eat normally in a week or so.
After your gums are healed, we can discuss implants, bridges or dentures as a way to fill the gap left behind by the removed tooth.
On top of these two treatment options, we may need to prescribe an antibiotic to clear any infection that you may have and pain management may be necessary. In all cases, treatment is a relatively quick fix that will impact your life for 3 - 7 days before you start to feel like yourself again.
Identifying and treating a dead tooth is a quick process. If you suspect that you have a dead tooth or that your tooth is in a severe state of decay, schedule an appointment with us. We’re more than happy to conduct a full dental exam and recommend the best treatment for you.